Pancreatic cancer survivor shares emotional treatment journey

As scary as receiving a cancer diagnosis is, having symptoms that keep getting worse without knowing the cause isn’t much better. And as scary as any cancer treatment might sound, it beats hearing, “There’s nothing else we can do for you.”
Amy Linville lived in both of those realities. She endured one journey that led to being diagnosed with pancreatic cancer, then another to find specialists who could treat it and offer her a chance at a long life. Her self-advocacy, determination, and faith led her to the UAB O’Neal Comprehensive Cancer Center, where she underwent what she calls a miraculous surgery to remove a dangerous tumor.
Pancreatic cancer accounts for just 3% of cancer diagnoses but is the No. 3 cause of cancer death in the United States. It is difficult to diagnose because its symptoms could indicate a variety of other conditions, and the tumors are not easy to spot on routine imaging scans. Also, it spreads quickly, and surgical removal of the cancer – the only way to destroy it – can be risky.
Confusing symptoms
Linville, 43 – a resident of Chattanooga, Tenn. – had several other difficulties on her way to being diagnosed with pancreatic cancer. A health care professional who manages a skilled nursing facility, Linville had just recovered from COVID-19 in fall 2021 when her blood sugar levels became alarmingly high. She was already managing thyroid disease, and her doctors thought the sugar spike could indicate diabetes. After all, some people suffering from “long COVID” also were being diagnosed with diabetes, they told her.
She began experiencing troubling symptoms following the high doses of insulin she had been prescribed. She lost weight rapidly, nearly 100 pounds. She developed a nearly constant pain in her abdomen and generally stopped feeling like herself. “I had to speak up about the way I was being affected and push for new information, because this was going in the wrong direction quickly,” Linville said.
Her local doctor performed a scan in February 2022 and discovered a large gallstone. This was a reasonable explanation for her symptoms. The gallstone removal required emergency surgery. She was encouraged that this might be the end of an ordeal, but it was a detour instead. Although her blood sugar improved briefly, the abdominal pain never stopped.
Early diagnosis
In June 2022, Linville’s blood sugar skyrocketed, and her endocrinologist agreed to the CT scan she had been seeking. It revealed a mass on her pancreas, and she was admitted to her local hospital immediately. “I had just recovered from the gallstone surgery, but the other symptoms had been constant for so long, I was just ready to face this down,” Linville said.
She was encouraged that the pancreatic cancer was caught in its early stages. And since she was unusually young to be diagnosed, she was prepared for her doctors to be as aggressive as possible with treatments.
However, her optimism came with some bad news. The tumor was dangerously close to a major vein and an important artery. This meant she would have to undergo chemotherapy prior to surgeons attempting to remove it. She underwent two types of chemo from July to October 2022.
The chemo killed the cancer cells but did not shrink the tumor. Radiation therapy was the next course of treatment, five days a week for six weeks. “I was willing to let them go as aggressive as possible again, just for a chance to have surgery,” Linville said. Over the next six weeks, the tumor shrunk, but not enough that her radiation oncologist had much hope for the surgery. This was in March 2023.
“I had done everything I could at this point, and I had persevered hopefully and faithfully, so I was going to live out my days peacefully,” Linville said, adding that having the conversation about dying with her children was more difficult than coming to terms with the reality in her own mind.
The next day, a surgeon from her local hospital called and offered her a ray of hope. He pointed her to the Pancreatic and Hepatobiliary Cancer Clinic experts at the UAB O’Neal Comprehensive Cancer Center, where she was scheduled for an appointment two days later.
A risk worth taking
At UAB, Linville first met with Vikas Dudeja, M.D., who recommended J. Bart Rose, M.D., for his experience in pancreatic surgery. Dr. Dudeja called Dr. Rose as the latter was getting in his car to leave for the day.
“They said mine was an urgent and unique opportunity; I had never seen doctors focus so quickly on a solution,” Linville said. “From the moment Dr. Rose came back from his car, I felt like I was the only patient they were thinking about. We recorded that whole conversation, and he said, ‘I’ll give you 30 seconds of what can go right and 35 minutes of what could go wrong.’ I didn’t come all that way to get a sugar-coated version. We were ready to act – or not. I wanted the whole picture.”
Dr. Rose gave her a 20% chance of her surviving surgery. He patiently took questions from Linville and her two college-age children who attended the appointment. They agreed with her reasoning that this was her one chance at a long and healthy life, and it was the best choice despite the risks. In the four weeks between that meeting and her scheduled surgery, Linville prepared for either outcome, and she quietly made end-of-life arrangements with attorneys and accountants.
The day of her surgery was far from the grim experience one might expect. “I was treated like a celebrity when I arrived at UAB on that Friday,” Linville said. “Doctors and residents who had come in on their day off were giving me pep talks, saying, ‘You’re getting the big-daddy surgery!’ I could just tell everyone was with me in this and so upbeat and even proud of me.”
‘Did they get it?’
Linville’s surgery took more than 10 hours. It required two blood transfusions, and 34 lymph nodes were removed from the area as a precaution. She regained awareness two days later in the Intensive Care Unit (ICU). Her first request (which she doesn’t remember) was for a dry erase marker. She couldn’t talk but wrote on a board, “Did they get it?” Nurses told her it looked successful and explained what had been accomplished. Still, she had another 48 critical hours in the ICU and was monitored there for a total of six days.
Linville was not expecting to wake up from surgery, and she now had a difficult road ahead. In one terrifying moment, a suture loosened, and she bled from her abdomen. Her nursing team reacted quickly, and she sensed the urgency as staff crowded around to help. Nurses later called a musician from UAB Arts in Medicine to bring a violin to her room and play soothing music to help calm her anxiety.
“I have high standards for care because it’s my job, too, but the way they coordinated extra care for me in the ICU was outstanding, above and beyond,” Linville said. One of the ICU nurses helped Linville manage her back pain in between pain pills by massaging her for up to two hours at a time.
Linville was released after several additional days at UAB Hospital, but her doctors warned her to prepare for a difficult and painful recovery. “Dr. Rose said, ‘It’s going to take all your energy just to get up, and you’re going to be exhausted for a while.’ Once again, that was something that I needed to know, because it was spot-on – I wouldn’t have believed it with my toughness and pain tolerance,” she said.
An emotional phone call
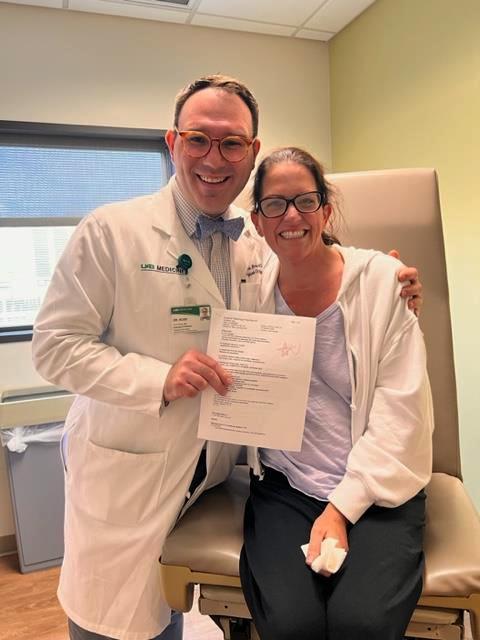
A few days after she returned home, Dr. Rose called her personally. According to Linville, he said, “I just wanted to give you the report myself. We got it all, Amy! All 34 lymph nodes are clear. It’s a miracle we got it all.” It was an emotional call between partners in a brave procedure. “That care team is not normal, the way they communicate so well up and down the ranks. Every call has been personal,” Linville said.
In August 2023, Linville underwent a follow-up scan and labs, which came back clear, and she’s due for another scan in December. Her blood sugar has remained normal, even though many people who have surgery for pancreatic cancer develop diabetes. She still experiences digestive issues, weight loss from the procedure, and pain during everyday activities, but Linville is back at work. She’s working with a personal trainer to build back her mobility and strength. And she is more thankful than ever for her ability to help others by sharing her story.
Linville has advice for those struggling through symptoms without a clear diagnosis or treatment path: “Advocate for your own health,” she said. “Sometimes it’s not going to be cut and dry. You have to trust yourself first to know your symptoms and gut feelings and know when you’ve found the experts to trust as well. Finally, try to look ahead bravely one step at a time with a peaceful heart – my faith has helped me do that.”
Click here to learn more about cancer care at the UAB O’Neal Comprehensive Cancer Center.




