Basic Science, Serendipity and the Road to Discovery
Story by Matt Windsor | Photos courtesy of Children’s of Alabama, UAB Medicine, the Bibb Lab and the UAB Archives
Cancer grows. That is its defining characteristic. Much of the work of basic science researchers in oncology is devoted to finding ways to kill or deactivate cancer cells – or to finding where they are hiding in the body, waiting to grow again.
Targeting any hostile organism ideally involves identifying a unique protein or molecule in the invader that is not present in the human. Otherwise, healthy cells will be killed or suppressed along with cancer cells. This is why chemotherapy drugs and radiation, while targeted in a sense, can bring debilitating side effects. They selectively harm quickly dividing cancer cells, but they can also harm healthy, quickly dividing cells in the scalp, gut and beyond.
The original wonder drug, penicillin, is so effective because it targets unique proteins that build cell walls in bacteria – proteins that are not present in human cells. Viruses, which rely on human cell machinery to grow and replicate, are a harder problem to solve. Cancer cells, which are human cells gone awry, are tougher still.
But over the past 50 years, basic science researchers in the UAB O’Neal Comprehensive Cancer Center have contributed to many breakthroughs in targeting cancer cells and viruses. Those breakthroughs have improved the lives of patients across Alabama and around the world, and investigators continue to break new ground in cancer science and translate those discoveries into clinic-ready therapies.
Going viral
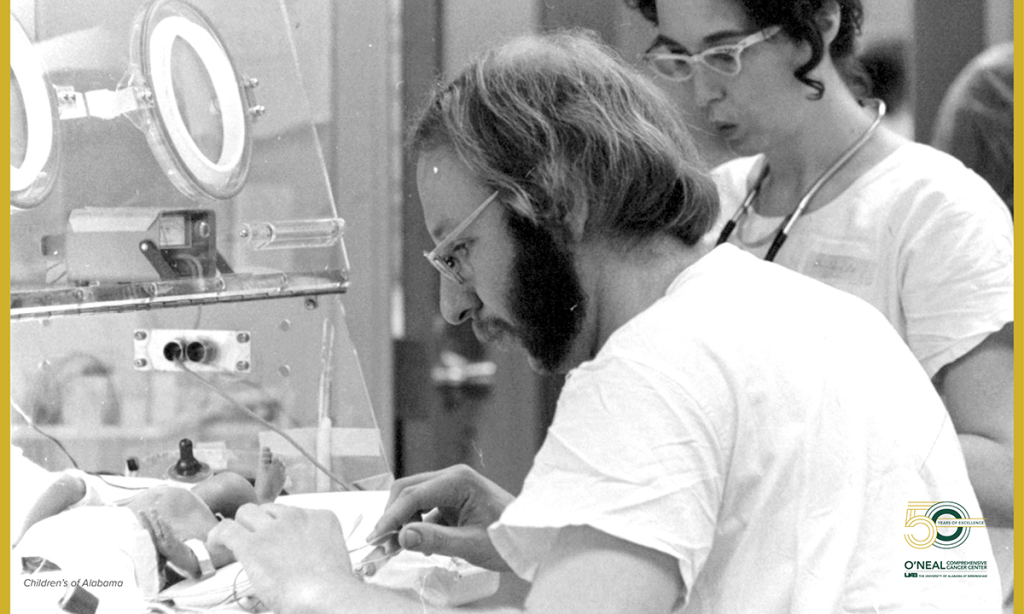
Richard Whitley, M.D., who is now a distinguished professor of pediatrics and the senior advisor for drug discovery and development at the O’Neal Comprehensive Cancer Center, came to UAB in 1970 to study with Charles Alford, Ph.D., who had built a national reputation for the university in infectious diseases research. Alford was a pioneer in the study of cytomegalovirus, or CMV, a type of herpes virus passed from mother to infant.
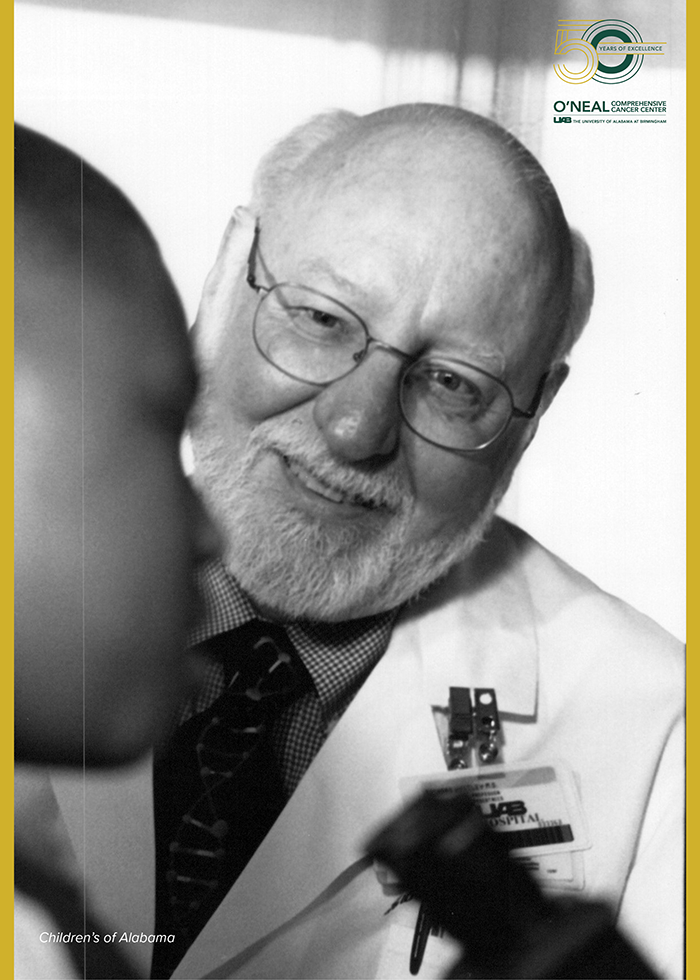
“That was in the very beginning, when John Durant had just applied to the National Cancer Institute to establish [an NCI-Designated] Comprehensive Cancer Center at UAB,” Whitley said. John Durant, M.D., was the first director of what became the O’Neal Comprehensive Cancer Center, serving in the position from 1970 to 1982, and was at the helm when the O’Neal Cancer Center received its first core grant and its first designation from the NCI.
Whitley became a leader in the study of herpes viruses, including herpes simplex virus, or HSV. HSV infects more than two-thirds of the population of the planet and is generally asymptomatic. But in patients with weakened immune systems – including cancer patients – it causes painful blisters and can lead to fatal encephalitis.
In 1977, Whitley and Alford demonstrated for the first time anywhere in the world that a virus infection – HSV in this case, in patients with encephalitis – could be successfully treated using an intravenous drug. The drug was vidarabine, developed at Birmingham’s Southern Research Institute, which targeted a specific enzyme produced by herpes viruses that is necessary for their DNA replication.
Vidarabine became the standard treatment worldwide for HSV and herpes zoster, which causes chickenpox in children and shingles in adults and is particularly problematic for cancer patients.
Whitley, Alford and UAB were also instrumental to the testing and adoption of acyclovir, a second-generation antiviral against herpes viruses. Today, antiviral drugs are used to treat COVID-19, influenza, HIV and many other diseases.
“The Cancer Center was the springboard of antiviral therapy,” Whitley said. “It worked out exceedingly well and we were able to enroll many patients in clinical trials.”
Whitley then had another idea, which emerged from a sabbatical in the lab of Bernard Roizman, Sc.D., at the University of Chicago. What if they could engineer a version of the herpes virus to selectively attack cancer cells?
In 1990, Whitley and Roizman identified a spot on the HSV genome, gamma 34.5, that was crucial to its ability to infect healthy brain cells. By blocking gamma 34.5, Whitley reasoned, they could create a virus that infected and killed cancer cells but left normal cells alone. Whitley believed this could be a way to attack hard-to-treat brain cancers, including the most lethal version, glioblastoma multiforme.
Whitley received a major grant from the National Cancer Institute to lead the study of oncolytic – that is, cancer-destroying – herpes viruses.
“We used these oncolytic viruses in animal models, and we had survival with no evidence of residual tumors,” Whitley said.
The work of refining these viruses for regular clinical use continues. Whitley’s longtime collaborator, James Markert, M.D., MPH, who serves as a senior scientist at the O’Neal Comprehensive Cancer Center and the chair of the UAB Department of Neurosurgery, leads the development of one promising virus candidate, G207, for treating brain tumors in adults. In a study published this year, Markert and other researchers reported that G207 appeared to boost immune response and improve overall survival for patients with glioblastoma in a clinical trial.
Gregory Friedman, M.D., an associate scientist in the Cancer Center and a professor in the Division of Pediatric Hematology-Oncology within the UAB Department of Pediatrics, also leads studies of G207 in pediatric brain tumors. In 2021, Friedman and his co-authors reported on a first-in-human trial of G207 in pediatric patients with aggressive brain tumors. The drug more than doubled median overall survival, from 5.6 months to 12.2 months, and four of the 11 patients were still alive 18 months after treatment.
Whitley is also the co-founder of the Alabama Drug Discovery Alliance, a partnership between UAB and Southern Research that combines each institution’s strengths in basic science research and drug development. The partnership’s pipeline includes promising drugs to treat multiple myeloma and adult relapsed leukemia.
“We are really making history at UAB,” Whitley said.
Engineering antibodies against cancer
The COVID-19 pandemic has made monoclonal antibodies a household word. These lab-created therapies, commonly known to scientists and physicians as Mabs, have the special ability to target very specific parts of cells or invading organisms. They are at the heart of the precision medicine revolution in cancer.

UAB researchers played a major role in taking Mabs from a laboratory idea to patients around the globe. The story starts with John Kearney, Ph.D., now a professor in the UAB Department of Microbiology and a senior scientist in the O’Neal Cancer Center. In 1977, Kearney, who had just joined the microbiology faculty, traveled to Germany to learn how to create monoclonal antibodies in the lab of Klaus Rajewsky, Ph.D. Kearney put in what he has called “backbreaking work” to find and isolate a cell line that could produce pure monoclonal antibodies for the first time. Kearney’s cell line “became famous worldwide instantaneously,” Rajewsky said.
Kearney brought the line back to UAB and taught many of his colleagues to make monoclonal antibodies. In 1983, Albert LoBuglio, M.D., who had been studying monoclonal antibodies at the University of Michigan, joined the Cancer Center as its second director.
“It seemed like an ideal time to put a team together specifically for monoclonal antibody studies,” LoBuglio told UAB News in 2017.
In 1987, UAB researchers carried out the first ever trial of a genetically engineered monoclonal antibody, and shortly afterward the Cancer Center received a major grant for monoclonal antibody trials. In 1994, its scientists carried out a novel trial that led to the FDA approval of rituximab, or Rituxan, a monoclonal antibody for non-Hodgkin lymphoma. And in 1995, the Cancer Center helped lead the successful trials of trastuzumab, or Herceptin, a monoclonal antibody used to treat breast cancer. To this day, the majority of the drugs being studied in Phase I clinical trials at UAB for cancer are monoclonal antibodies.
Targeting troublesome pathways
As cancer therapies become more targeted, there is a corresponding need to identify the specific patients who will benefit from each one. Researchers have discovered that the same type of cancer can be driven by any one of several different chemical pathways in the body, even if they are linked to the same genetic mutation.
“Many times, the mutations trigger downstream pathways that have to be understood,” said James Bibb, Ph.D., who serves as a professor and the vice chair for basic research in the UAB Department of Surgery and as a senior scientist at the O’Neal Cancer Center.
“If we can identify multiple pathways that all contribute to cancer, we can target important nodes” controlling these pathways, Bibb explained.
One of these nodes is cyclin-dependent kinase 5, or Cdk5, which is an enzyme that regulates the development of the central nervous system and plays a role in cognitive processes such as learning and memory. About a decade ago, Bibb’s lab developed an animal model in which they could turn Cdk5 production on and off.

They wanted to use it to study neurodegeneration in Alzheimer’s disease. Instead, the researchers found that boosting Cdk5 created medullary thyroid carcinoma, a form of neuroendocrine cancer.
Neuroendocrine cells control metabolism and respond to environmental signals in organs such as the thyroid and pancreas. There are limited treatment options for neuroendocrine cancers, and mortality rates have not improved in decades. This is partly because no one had been able to create effective models of the disease in animals — until Bibb’s accidental discovery.
“We’ve studied Cdk5 now in various kinds of neuroendocrine cancer,” Bibb said. “A large proportion, perhaps half, of neuroendocrine cancers are driven by Cdk5.”
Which ones? In a 2020 paper, Bibb and his co-authors reported that several elements of signaling pathways activated by Cdk5 could be used as biomarkers. Tumors with these pathways activated were responsive to experimental anti-Cdk5 drugs now in development, and tumor growth was halted. Bibb’s lab is now developing a novel anti-Cdk5 drug of its own.
In January 2022, Bibb received $1.2 million from the Neurendocrine Tumor Research Foundation’s Accelerator Award program to continue his work on anti-Cdk5 treatments and biomarker tests.
“Cdk5 has also been strongly linked to colorectal cancer,” Bibb said. “And it is implicated in features of melanoma and also glioblastoma.”
Bibb, who joined UAB in 2016, is interested in cognition, mental illness and neurodegeneration, in addition to cancer. Cdk5 also has the potential to improve cognition and to serve as a target for depression treatment.
“I am a neuroscientist who became a cancer biologist as well,” Bibb said. “I came to UAB because this is a great opportunity to work at the nexus of cancer and neurobiology. The O’Neal Comprehensive Cancer Center has been the perfect environment to conduct this research.”
A new area of research for Bibb’s lab is in the neurological effects persisting in patients after chemotherapy. Some 70-80% of patients report cognitive issues after chemotherapy, including a troubling fuzziness of thinking known as “brain fog.” Here, too, Cdk5 seems to play a role.
“We are taking a broad, exploratory approach,” Bibb said. “What’s happening to the immune system in the brain and specific circuitry? We are applying the most advanced neuroscience techniques to this problem.”
An expanding role for imaging agents that find and treat cancer
One of the workhorse tools in cancer care today is PET, or positron emission tomography, imaging. PET is often used to look for metastasized cancer cells that have spread in a patient’s body. PET does this with radiopharmaceuticals – lab-created compounds that both emit positrons, which the PET camera can detect, and can home in on a particular biological feature. The most common radiopharmaceuticals used in oncology seek out glucose because cancer cells consume far more glucose than normal cells. But this trick does not work for all cancers, and sometimes the most important information is not just where a cancer cell is, but what it is doing. The field is expanding rapidly in search of new radiopharmaceutical tools.

Making radiopharmaceuticals requires a cyclotron, a machine that spins to generate a stream of protons that can turn elements such as oxygen and fluorine into briefly radioactive (positron-emitting) versions of their normal selves. The 24 megaelectronvolt (MeV) cyclotron in the basement of the Wallace Tumor Institute can make all the traditional PET radiopharmaceuticals, as well as experimental radiopharmaceuticals that can be used in new PET scans. But it is the team built and led by UAB Cyclotron Facility director Suzanne Lapi, Ph.D., that is cementing UAB’s national reputation in this cutting-edge field.
“My group is looking at how to make the building blocks for new radiopharmaceuticals and new imaging agents,” said Lapi, who is a senior scientist at the O’Neal Comprehensive Cancer Center and the co-leader of the center’s Experimental Therapeutics Research Program. In November 2021, UAB joined the U.S. Department of Energy’s University Isotope Network to produce isotopes focused on advancing scientific research.
“We ship these isotopes all over the United States and Canada,” Lapi said.
One area with a great deal of promise is known as theranostics, which are tools that can be used both to diagnose disease and to treat it. One theranostic recently approved by the FDA is the NETSPOT-Lutathera combination, which targets the somatostatin receptor present on neuroendocrine cancers.
“If the person’s cancer lights up on the scan, we know that they are somatostatin-receptor-positive,” Lapi said. “We can image the whole person to find cancer cells anywhere in the body.”
That is NETSPOT’s job, Lapi explains.
“Then we can use a therapeutic isotope [Lutathera] that delivers lethal radiation to those cancer cells,” she said. “And we know from the imaging study that the therapeutic will be effective.”
Thanks to the cyclotron, “UAB was the first site in Alabama to use NETSPOT-Lutathera, and we continue to be one of the highest-volume sites in the country,” Lapi said. “UAB is getting a name in the theranostics realm, bringing agents into clinical trials here.”
Benjamin Larimer, Ph.D., an assistant professor in the UAB Department of Radiology and associate scientist at the O’Neal Cancer Center, joined UAB in 2019. Larimer cites the UAB Cyclotron Facility and the opportunity to work with Lapi as two of the main reasons for his move to UAB.
“The reputation that Suzy has means that many companies come to UAB with new therapeutics, and that means patients in Alabama have access to cancer-fighting drugs well before they would be able to access them otherwise,” Larimer said.
Larimer’s research focuses on finding diagnostic techniques that can help clinicians decide when patients may benefit from immunotherapy treatments. These treatments have been remarkably successful, even curative in some cases, but the majority of patients do not respond to immunotherapy. Potential side effects and high costs mean many clinicians are hesitant to use immunotherapy.
“It can take six months to a year with current methods before you really understand if you are getting any benefit, and in cancer, you always want to treat as quickly as possible,” Larimer said.
But Larimer is studying one way to get a faster readout: a radiopharmaceutical targeting granzyme B, which the immune system uses to kill dangerous cells such as tumor cells. He says a first-in-human clinical trial has had encouraging early results.
“In patients who have responded to immunotherapy, we see an increase in the PET signal of their tumor in as early as six weeks,” he said.
Larimer is also working with Anna Sorace, Ph.D., assistant professor in the UAB Department of Radiology and associate scientist at the O’Neal Cancer Center, to make nonresponsive tumors susceptible to immunotherapy. In a study published this year, Sorace and Larimer used a radiopharmaceutical called FMISO, which is trapped in cells with no oxygen, combined with a drug called evofosfamide, which kills these hypoxic cells. In animal models, the researchers were able to achieve responses equivalent to non-hypoxic tumors. Sorace is now starting a clinical trial of FMISO-evofosfamide in patients with triple-negative breast cancer.
“If the mechanism of hypoxia is conserved across species, then 18F- FMISO can serve to guide the timing of evofosfamide in personalized and image-guided adaptive immunotherapy trials,” Sorace and Larimer told UAB News in October 2021. “Both 18F- FMISO and evofosfamide have been approved as investigational new drugs by the United States Food and Drug Administration, and therefore, rapid clinical exploration is possible to test the translation of our described paradigm. If successful, this strategy may act to rescue otherwise non-responsive tumors and enhance the number of patients who benefit from immunotherapy.”
With regard to the future, Lapi considers the impact of advancements in imaging for precision medicine and oncology.
“There is a great deal of excitement around the potential of imaging and its role in expanding precision medicine therapies to more cancer patients,” Lapi said. “[O’Neal Cancer Center Director] Barry Sleckman is very supportive and we have enthusiastic partners in oncology.”




